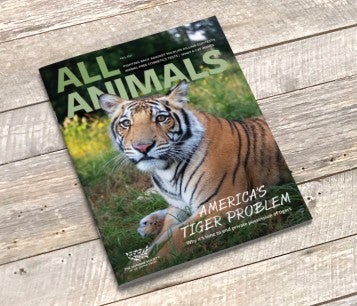
All Animals, our award-winning magazine, is packed with stories about how your donations are changing the world for animals. Inside each issue, we give you the latest on how you're helping us fight for all animals, as well as profiles of people on the front lines, tips for caring for your pets and protecting wildlife, heartwarming tales of rescue and rehab, actions you can take and more. Beautifully illustrated and thoroughly researched, All Animals will inspire you and keep you informed on the issues you care about.
Donate $25 or more and receive a free subscription to All Animals magazine.
HumanePro is our dynamic, comprehensive online resource for those in the trenches of animal care. Through news, trainings, how-to guides, job and grant directories and our annual Animal Care Expo, we help animal shelters, rescue groups and other animal welfare professionals support pet owners in their communities and save more animals.

Supporters share their favorite photographs and love of animals with All Animals magazine. View the latest featured photo and learn how to submit your own!